13-9, 2 Rio Tower, Persiaran Rio, Bandar Puteri, 47100 Puchong, Selangor, Malaysia.
Acute Stress Disorder Criteria: A Guide to Early Diagnosis and Healing
- On
- InUncategorized
Stress is part of daily life — from tight deadlines to personal conflicts — but Acute Stress Disorder is very different. So, what exactly is acute stress disorder? It is not about everyday worries; rather, it is the immediate reaction of the mind and body to a traumatic event. Imagine a car accident, a sudden loss, or being caught in a natural disaster. In these moments, your nervous system goes into survival mode.
It is common to feel anxious, struggle to concentrate, or notice physical changes such as a racing heart, sweaty palms, or disrupted sleep after a traumatic experience. Some people may even feel emotionally numb, detached, or as if they are watching life from the outside. These are the body’s ways of coping with overwhelming experiences.
Acute stress disorder and Post-Traumatic Stress Disorder (PTSD) may sound similar, but the difference lies in timing. Acute stress disorder develops within the first month after a traumatic event and lasts from three days up to a month. PTSD, on the other hand, is diagnosed when symptoms persist for more than a month or even appear later.
While some short-term stress is normal after trauma, it is important to recognise when it crosses into acute stress disorder. Understanding its signs and criteria can help you know when professional support is needed — and when healing can begin.
Breaking Down the Acute Stress Disorder Criteria
Mental-health professionals use the DSM-5, the standard diagnostic guide, to diagnose acute stress disorder. Its criteria include:
- Exposure to trauma: The person has directly experienced, witnessed, or learned about a traumatic event involving serious injury, threat, or death.
- Intrusion symptoms: Distressing memories, flashbacks, or nightmares that replay the trauma.
- Negative mood: A lasting inability to feel positive emotions, such as joy, hope, or love.
- Dissociative symptoms: Feeling disconnected from yourself (depersonalisation) or your surroundings (derealisation).
- Avoidance behaviours: Actively steering clear of reminders, whether it’s places, people, or conversations linked to the trauma.
- Arousal and reactivity symptoms: Heightened startle response, difficulty sleeping, irritability, or being constantly “on guard.
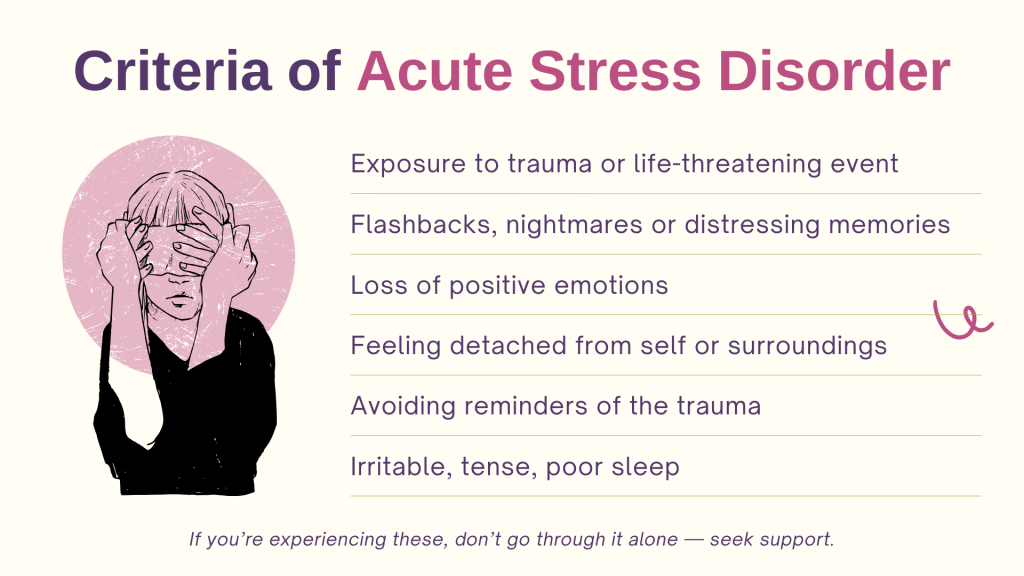
📌 Important timeline: These symptoms must develop within 3 days to 1 month of the traumatic event. If symptoms persist longer than a month, the condition may shift toward PTSD.
By understanding the criteria, clinicians can use these criteria to guide early trauma assessments and help individuals access timely support.
Why Understanding These Criteria Matters
Recognising the signs of acute stress disorder early can make all the difference. Left untreated, acute stress disorder may progress into PTSD or contribute to other mental health challenges such as anxiety and depression. The sooner you recognise those signs, the sooner healing can begin.
Unfortunately, many people dismiss their experiences — writing them off as “just stress” or fearing the stigma of seeking help. Knowing the official criteria helps validate these feelings: what you’re experiencing is real, and it deserves care.
The good news? Acute stress disorder is often very responsive to early treatment. With early intervention, therapy, and coping strategies, most people regain balance and prevent long-term complications. A professional trauma assessment plays a critical role, helping mental health providers design a personalised care plan suited to your needs.
The Role of Trauma Assessment in Early Diagnosis
A trauma assessment is often the first step toward healing. It’s not about labels — it’s about clarity and direction. Assessments may include:
- Clinical interviews: Guided conversations with a professional to explore your experience and symptoms.
- Symptom checklists: Tools to measure intensity and patterns of trauma-related reactions.
- Psychological screening: Utilise evidence-based questionnaires to understand how trauma is impacting your daily life.
Importantly, trauma assessments are conducted with compassion and confidentiality. They are designed to make you feel safe while offering insights that guide your recovery.
Everyone’s brain and body respond differently to trauma. You do not have to figure it out alone. Rather than self-diagnosing, let a professional use a specialist tool to tailor treatment for you. Think of an assessment as a map: it shows where you are and helps you plan possible next steps.
Take the First Step Toward Healing
Acute stress disorder does not define you. It’s a temporary response to trauma. Recovery is very possible, especially with early support. The key is not to wait. The earlier you address symptoms, the more effective your healing process will be.
If you or someone you care about may be experiencing symptoms of acute stress disorder, reaching out is the first step toward healing. At Skybi, we provide confidential, expert-led Acute Stress Disorder Assessments to help you understand what you’re going through and explore the right next steps for recovery.
Need Help? Start with a Professional Trauma Assessment.
💬 Contact us on WhatsApp — our team is here to support you, every step of the way.
written by Wei Xin on 19 September 2025







